The University of Navarra Clinic It has been positioned for decades as one of the reference centers in highly complex medicine, research and teaching, a triangle where technology is no longer a support, but a structural piece of the care model. In this context, the role of the Systems area goes far beyond infrastructure maintenance; it’s about align digital strategy with clinical and academic strategysupporting high-performance teams that work closely with doctors and researchers.
Josep Maria Gostco-CIO of the Clínica Universidad de Navarra, summarizes this idea well by remembering that “the IT strategy must be the strategy of the organization”, something that in health translates into decisions that directly impact the diagnosis, treatment and patient experience.
In this interview we delve into how the Clinic is using Big Data and AI to accelerate clinical research, especially in identifying candidate patients for more than 500 open trials and validating the real leadership capacity of those studies. The combination of language models (LLM), structured and unstructured information, genetic data and medical images opens the door to more personalized medicine, but also poses enormous challenges of interoperability and data governance.
Josep María Gost insists that the future lies in systems that “speak the same language” and allow secure queries regardless of the origin of the data, something critical when collaborating with other research centers.
Another of the key axes is the deployment of generative AI and specialized agents, the result of a strategic alliance with Microsoft and the creation of an internal AI unit within the Systems department itself. More than ten agents already support tasks such as writing reports, searching for clinical guidelines or synthesizing information, while the Clínica Universidad de Navarra continues to support AI in diagnosis. An example of this is the pathological anatomy department, which has been completely digitized to incorporate AI algorithms, becoming a European benchmark.
Of course, under a clear premise: all AI output must be validated by a specialist and each project is submitted to an AI committee where medical, legal and technology sit to ensure safety and regulatory compliance.
(MCPRO) The University of Navarra Clinic is a benchmark in highly complex and innovative medicine. What main challenges do you face when digitally transforming the organization, and how does the IT area articulate a strategy capable of balancing research, clinical excellence and teaching?
(Josep Maria Gost) In the Clinic the level of demand is very high. Our professionals combine assistance, research and teaching, and expect technology to be up to par. From the Systems department we not only respond to your needs, but we seek to anticipate, identifying disruptive opportunities that add value.
As I heard on one occasion, “the strategy of the IT area must be the strategy of the organization,” and I fully share this vision. We have specific plans in digitalization, architecture and cybersecurity, but all of them are aligned with the Clinic’s global strategy and are continually reviewed with those involved. To achieve this, we have incorporated figures such as Business Partners, who connect technology and business.
Our greatest challenge is to maintain high-performance teams, cohesive with the healthcare and research areas, to continue promoting digital transformation without losing focus on clinical excellence.
(MCPRO) Digitalization is accelerating health research. How are you applying technologies such as Big Data or AI in medical research projects within the Clinic?
(Josep Maria Gost) We are exploring multiple lines to help our researchers with the new possibilities that these technologies offer us.
In the field of clinical trials, it is key to identify if a patient is a candidate to participate. To do this, we use solutions that combine Big Data and AI, capable of analyzing the patient’s characteristics and cross-referencing them with available trials, both our own and external, thus offering options that can benefit the patient.
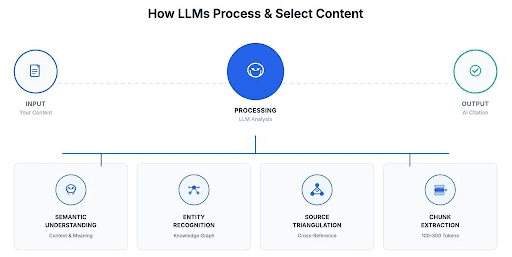
On the other hand, the Clinic carries out a significant number of trials; At this time we have more than 500 open, of which it is essential to know the capacity to be able to lead them with a sufficient number of candidate patients. Until recently, these validations were based on NLP (natural language processing), but with LLM models we can obtain more agile and precise responses.
In addition, we are promoting projects that integrate structured and unstructured information, genetic data, medical images and other relevant elements. This is one of the great challenges for the coming years.
Finally, secure collaboration between research centers is essential. We are advancing tools that integrate multimodal information under a strict regulatory framework, which reinforces the importance of interoperability, that is, that systems “speak the same language” and can respond to queries regardless of the origin of the data.
(MCPRO) You have signed an agreement with Microsoft to deploy generative AI in administrative and clinical tasks. What advantages does AI provide in the personalization of treatment, diagnosis and treatments for patients? What learnings and barriers do you highlight after the first pilot projects in the clinic?
(Josep Maria Gost) The advent of generative AI and the ease of creating models has opened new opportunities to improve patient care and optimize internal processes. Faced with this reality, we decided to create a unit specialized in AI within the Systems department and establish strategic alliances with technological partners such as Microsoft that are helping us both in training in the safe use of AI and in the development of solutions.
We currently develop more than ten AI agents aimed at tasks such as writing reports, searching for clinical guidelines and summarizing information. At the same time, we continue to invest in AI applied to diagnosis, betting on platforms that allow models from different manufacturers to be integrated. A notable example is the implementation of algorithms in pathological anatomy, possible thanks to the complete digitization of the department, which has made us a European benchmark.
All of these projects seek to provide medical and nursing staff with tools that increase efficiency and quality of care. It is important to emphasize that the information generated by AI must always be validated by a specialist. Initiatives such as the “virtual scribe”, which speeds up the writing of reports without interposing physical barriers between doctor and patient, are improving the care experience.
We are working to quantify the real impact of these solutions on patient care and administrative efficiency. In addition, each project goes through an AI committee that includes doctors, legal experts and the Systems department, guaranteeing security and regulatory compliance.
(MCPRO) The doctor-patient relationship is changing with technology. How are you innovating in the “patient journey” using new tools to accompany, inform and give rights to the patient throughout the care process, and what role does the vision of IT play in this journey?
(Josep Maria Gost) The “patient journey” is our reason for being and has always been a priority. Over time, this route has expanded; Initially we focused on offering clear information during the stay at the Clinic, especially in a high-resolution center where the patient moves frequently.
Today we work to prepare each visit and reduce unnecessary time, anticipating any clinical or administrative problem. In addition, we are implementing remote monitoring models. For example, this year we have integrated a tool into our app to monitor patients with vestibular migraine. Our digital architecture allows everything from basic monitoring to advanced solutions that facilitate continuous contact with specialists, reinforcing patient support.
However, it is important to take into consideration that there are less digital patients, so we have to be able to give them traditional alternatives to guarantee quality support.
(MCPRO) The management of sensitive data, such as medical records, is critical in healthcare. What are the biggest challenges and current priorities in cybersecurity and data protection? What model do you follow to ensure regulatory compliance, confidentiality and resilience against possible incidents?
(Josep Maria Gost) Security and data protection are a top priority. Our patients trust us with their most valuable data, and we must guarantee its protection. As they say, “security is like health: you only value it when you lose it”, which is why we take care of it proactively.
We have good governance bodies and policies, and we have invested in all lines: attack prevention, early detection and rapid recovery plans to ensure the integrity of the information. Total security is impossible, but we work with leading solutions and highly specialized teams.
We have had ISO 27001 certification for years and we are moving towards ENS. These certifications, although not mandatory for private entities, reflect our commitment to the highest security standards.
(MCPRO) Looking forward, what technological trends do you think will have the greatest impact on healthcare medicine in the next five years? Is there any disruptive technology on the Clinic’s strategic agenda that you can tell us about and that will help redefine the sector?
(Josep Maria Gost) The natural response is Artificial Intelligence, and in our case we are no exception. It will be revolutionary, especially in diagnosis and personalized medicine, adapting treatments not only to the disease, but to the genetic characteristics of the patient. However, success will depend on using it humanely: technology should never replace the support of the medical and nursing team.
On the other hand, we will see an increase in collaboration between hospitals and research centers, driven by platforms that allow large volumes of biological data (omics data) to be processed massively. This will open the door to personalized medicine that has yet to be exploited.